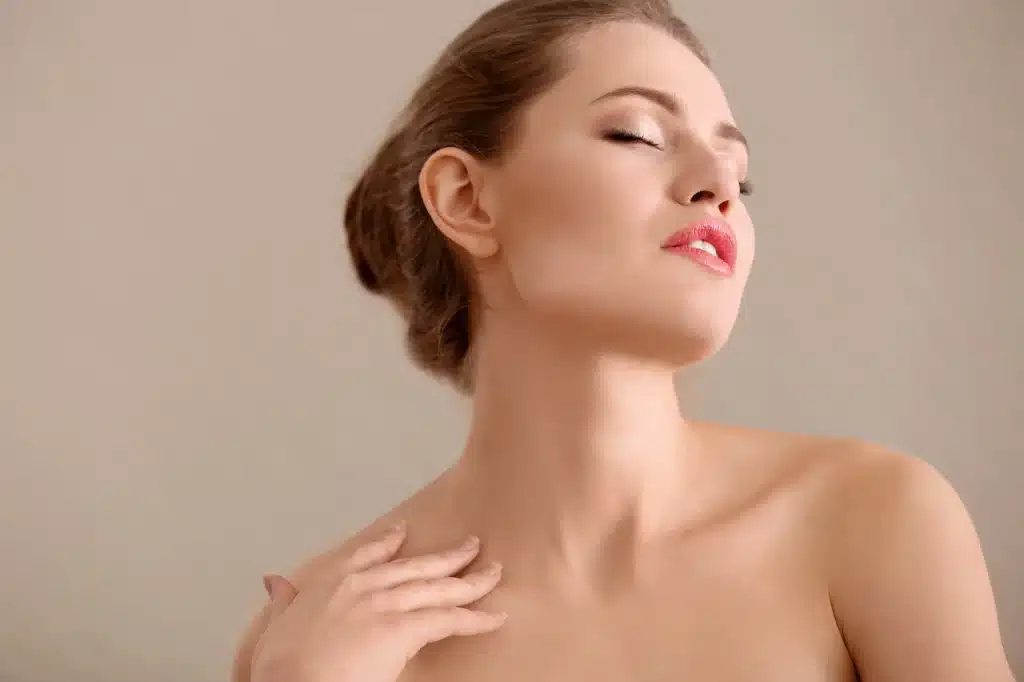
The location of the tear trough makes it an incredibly prominent feature on the faceafter all, the eyes are the windows to the soul. As such, deformities in this area (such as dark circles and puffiness) can be incredibly concerning to patients of all ages.
Generally, these issues are caused by the hollowing of the infraorbital region. Luckily, they can be treated using dermal fillers such as Fillmed, though this requires a high level of practitioner skill. In order to properly carry out this procedure, the injector must have a high degree of knowledge on the anatomy of the tear trough, as well as dermal filler rheology. Additionally, they must have experience in performing these injections, as improper delivery can result in a multitude of serious adverse effects. This being said, when properly carried out, these procedures can reduce both dark circles and puffiness, giving patients a refreshed, more youthful appearance.
Tear trough deformities
First discussed by Flowers in 1993, tear trough deformities are defined as periorbital hollows that extend obliquely from the medial canthus to the mid-pupillary line. This concern is primarily the result of aging, though it may affect patients of all ages. As the body grows older, the orbital septum weakens, which causes the lower lid fat pads to prolapse. The subsequent descent of suborbicularis oculi fat and orbicularis muscle exposes the orbital rim, leading to the formation of sagging under-eye skin and dark circles.
Today, the Tear Trough Rating Scale (TTRS) allows medical professionals to measure tear trough deformity. Through this method, doctors may examine the volume of prolapsed fat, amount of wrinkles, and level of hyperpigmentation in the under-eye area. Additionally, these markers allow practitioners to elucidate realistic treatment results to patients, which is imperative in achieving optimal procedural outcomes.
Approach to treating tear trough deformities
A 28-year-old female patient was complaining of dark circles under her eyes. She had no history of any medical or surgical conditions, and had no allergies or hypersensitivities. Previously, she had used over-the-counter creams to treat her dark circles, but had experienced no improvement.
Upon examination, she was found to have mild to moderate tear trough deformity with the presence of a palpebromalar groove. A degree of hyperpigmentation was also found in the skin inferior to the eyes, which she was told could not be corrected with dermal fillers.
Overall, she was an ideal patient to be treated with dermal fillers, which could correct the concern. While her hyperpigmentation could not be treated with this method, she was given other options for rectification of this issue.
A multitude of choices for dermal fillers were available for use world-wide, however, Teosyal Redensity II was ultimately chosen. This formula, uniquely, has low hygroscopic behavior due to the mixture of cross-linked and non-crosslinked HA together at concentrations of 15mg/g, which is excellent for procedures on areas where there is thin skin tissue. The chances are lower it will facilitate edema around the periocular area, after injection, when compared to other dermal fillers.
First, the palpebromalar groove was treated with a small bolus injection. The needle was directed 0.5cm adjacent to to the lateral canthus, and injections were repeated inferiorly along the groove. For this particular area, the needle was placed deep into the internal aspect of the orbital septum for volumization. Approximately 0.1ml of filler was used on each eye.
After this, the tear trough deformity was corrected. A 25-gauge cannula was inserted deep into the suborbicularis oculi fat, about 1cm away from the end of the tear trough. Though many authors would suggest a supraperiosteal injection, Teosyal Redensity II enables a more superficial placement without excessive edema formation. As such, the filler was gently placed in an intermittent retrograde micro bolus technique following the length of the deformity at the level of the orbital rim. The eye was protected by the index finger of the non-injecting hand above the orbital rim. The product was coaxed into the hollow with a gentle upward massage, helping the injector to avoid vascular structures. About 0.4ml of dermal filler material was used for each eye, totaling about 0.8ml for both eyes.
After treatment, the patient’s tear trough deformity was resolved. Due to the temporary nature of this treatment (Teosyal Redensity II is known to last for approximately 1 year), the patient needed to return for follow-up injections to maintain her results.
Conclusion
Correcting the tear trough deformity is a complex but rewarding process. It requires high practitioner skill, as this sensitive area is likely to experience severe side effects (such as blindness and skin necrosis) if done improperly. However, if done right, it can improve the self-confidence of any patient, improving their overall quality of life.