Periocular dermatochalasis, the term for under-eye bags and excessive loose skin surrounding the eye. This physical blemish occurs when the upper eyelids lose the youthful elasticity, enabling the formation of a “hood” of skin tissue that droops outwards and downwards onto the eyelashes. This obstructs the visual field of a patient and could cause discomfort. It also contributes to the formation of wrinkles on the eyelids.
This excessive skin and subcutaneous tissue is either caused by constant swelling (blepharochalasis), or aging and hereditary reasons. Other medical causes may include renal failure, trauma, thyroid eye disease, Ehlers-Danlos syndrome, hereditary angioneurotic edema, amyloidosis, and xanthelasma.
Symptoms of dermatochalasis
Indications for Surgery
In 2011, a report by the American Academy of Ophthalmology suggested that significant improvement in the vision, visual field, and quality of life in patients with this condition is associated with blepharoplasty. The pre-operative symptoms that can be resolved may include visual strain, superior visual field defect, down-gaze ptosis, and reduced upper margin reflex distance (distance central pupil reflex to edge upper lid margin).
Associated Periorbital Changes
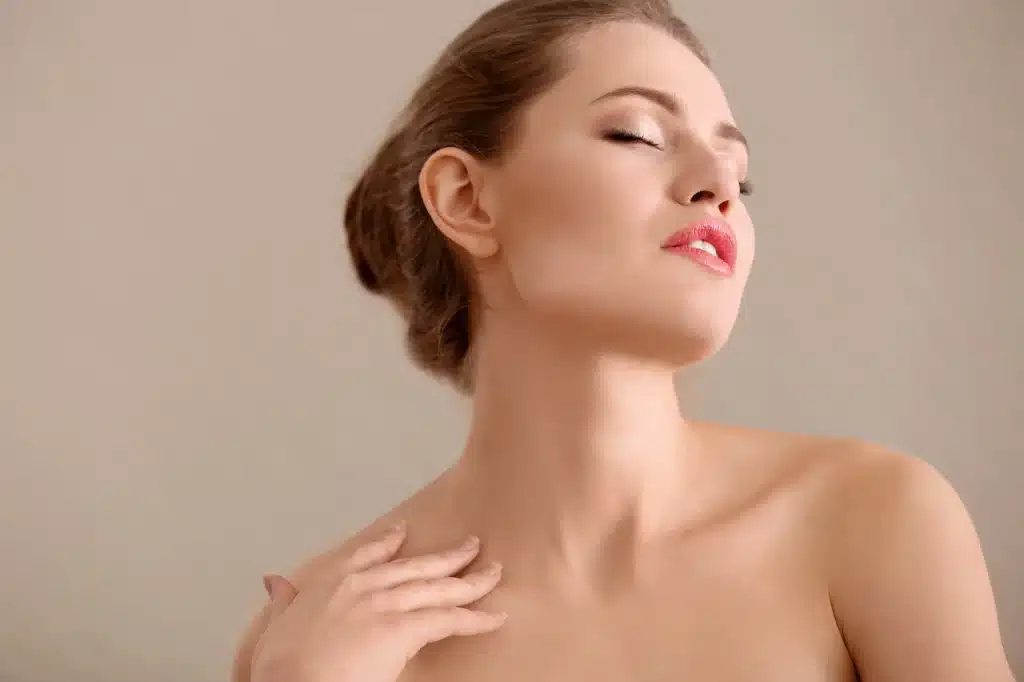
Dermatochalasis may be linked to eyelid ptosis. Additionally, the eyebrows may begin to sag, requiring compensatory eyebrow skin and soft tissue elevation.
Cosmetic Complications
Other than its effects on the vision, dermatochalasis may also create difficulty in applying cosmetics: the newly created hood disturbs the appearance of the normal upper eyelid pretarsal. Moreover, mascara can run due to constant contact with the upper lid lashes, as well as due to constant tearing of the eyes.
Management of Dermatochalasis Assessment
Like most procedures, assessment of the patient’s concerns, eyelids and the procedural plan is crucial in developing the correct surgical approach. Due to the extra tissue around the eyes, patients may complain about perpetually tired or sad eyes. Inquire how the eye bags affect them and determine if it affects the vision or cosmetics of the eye. You may take photographs for differentiation.
Other questions that can improve the investigation may include dry eye, history of corneal refractive surgery, or causes for blepharoplasty revision.
Physical examination of the eyelids, periorbital area and eyes
Physicians should examine the patient’s entire face, eyelids, and ophthalmic conditions at the beginning of the procedure. Assess the loose tissue and determine if there is co-existent eyebrow or eyelid ptosis or brow compensatory elevation. Inspect for fat herniation or protrusion. The small medial fat pad is often found herniating forward. Centrally, the pre-aponeurotic fat pad forms a fullness that holds up the skin fold. The sub-brow fat or ROOF (retro-orbicularis oculi fat pan) may descend centrally because of loose connective tissue and create a bulging effect.
To detect ptosis, measure the vertical palpebral aperture in mm through the level of the pupil as well as the upper margin distance in mm. Normal readings would indicate the upper eyelid margin resting at 3.5 to 4.5mm above the center of the pupil. Ptosis and blepharoplasty surgery should be considered if there is less than 2.5mm aperture.
Alternatively, 1 drop of 2.5% phenylephrine may be instilled into 1 eye to reveal any ptosis. This test will raise the eyelid and reveal its “normal” position in most patients. Another cosmetic consideration is the height of the supra-tarsal crease exerted by the levator aponeurosis pull, which is usually 7-9mm above the lid margin in women and 6.58mm in men.
Visual Field Analysis and Photography
Technological advances have allowed for computerized visual field tests to help gauge the extent of visual impairment. These tests may include Humphrey Field Analyzer test or the Binocular Esterman. The latter a gold-standard for measuring binocular visual fields for driving. By using Binocular Esterman visual fields, the physician can detect if the upper eyelids are interfering with the superior visual field, and if dermatochalasis causes a functional problem. Photographic documentation can also be helpful and should be taken with the patient in primary gaze or 30 degrees downgaze, oblique and in both side views before and after the procedure.
Goals of upper eyelid blepharoplasty
The trend on volume preservation along the lateral upper lid-brow complex while still maintaining a very natural look has been on the rise since the last 15-20 years. Upper eyelid blepharoplasty can help to create this sculpted upper lid with a visible pretarsal strip without any excessive lumps. The procedure creates high skin creases with a hollow upper lid as a response to overaggressive fat resection, all while preserving periorbital fat.
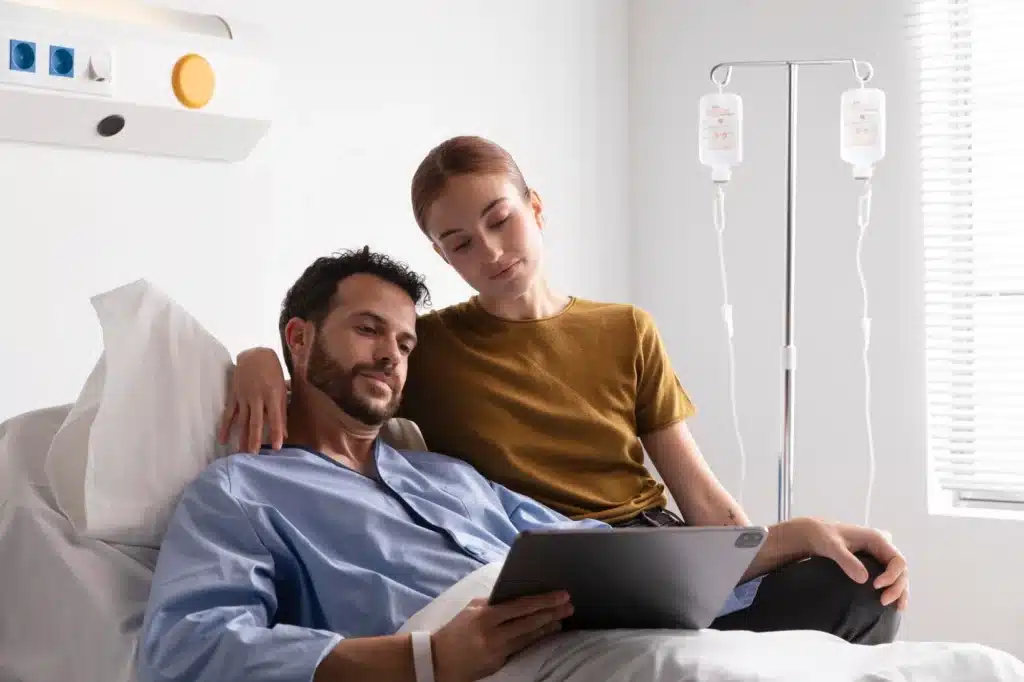
Treatment and Consent for Patient Expectations
Like any other aesthetic surgery, it is important to request the patient’s consent prior to treatment. They are obligated to understand the full process of the surgery, precautions, risks and expectations that are realistic. This consent form should be signed before surgery.
How to Perform Upper Eyelid Blepharoplasty
Indicate the skin crease
Prior to administering the local anesthetic, mark the skin crease while the patient sits upwards. The marking’s height varies between 6 and 8 mm. For Asian patients, the height is commonly lower as they have naturally low skin crease, with men having lower markings compared to women. There should be a minimum of 20 mm of skin remaining after the mark-up.
Local anesthesia
This is an important step to ensure full comfort in the patient. Inject a mixture of long-acting and short-acting anesthesia with a weak adrenaline level of 1 in 400,000. Each injection should be approximately 5ml, but adequate top-ups during the surgery are permissible. You may also use topical anesthetic drops on the eyes prior to and during the surgery. It is also advisable to wear a protective contact lens.
Incision
Make an incision a few millimeters above the eyelashes. It should follow the pre-marked lines and run along the natural eyelid skin crease.
Excision
Using a blade or a Colorado needle, remove an elliptical piece of skin and muscle in 2 separate layers. This greatly improves the surgery’s cleanliness with a lower risk of bleeding. Take great care to avoid injuring the underlying thin levator aponeurosis.
Sit the patient up
In order to check the eyelid appearance, you may sit the patient up several times during the surgery.
Managing the upper eyelid fat
Reduce the underlying medial fat pad or reposition it into the medial compartment to lessen its bulge. This repositioning may aid central sulcus volume.
One of the methods to shrink the fat pads is via bipolar coagulation-assisted orbital (BICO) septoblepharoplasty. The exposed and unopened orbital septum is corrected using bipolar coagulation, as opposed to excision. It is recommended, if possible, to preserve the fat to lower the risk of A frame deformity (deep central sulcus), which creates an aged look.
Closure
Use delicate absorbable or non-absorbable sutures and/or fibrin adhesive to close the skin incision.
Post-operative management
Patients are advised to instill lubricant drops 4 times a day for at least 1 week following this procedure. They may use ice packs over the eyelids and should increase the height of pillows they sleep on to reduce swelling. Sutures can be removed 7-10 days after the surgery. However, if fibrin adhesive is used, advise patients to protect their eyelids at night using plastic shields.
Adjunctive surgery for drooping brow ptosis
It is possible to perform a drooping brow ptosis or eyelid ptosis while correcting dermatochalasis.
Complications of Upper Eyelid Blepharoplasty Surgery
Inadequate assessment, poor surgical decisions and unmet expectations are some of the causes for complications of upper eyelid blepharoplasty.
- Mild bruising and swelling may last up to 3 weeks.
- Blurred vision may last for a few hours or overnight. The drying ocular surface is an effect of the anesthetic. If it persists for more than 24 hours, patients should seek immediate help from an oculoplastic surgeon.
- Watery eyes may occur for 1 or 2 days as reflex tearing to mild ocular discomfort.
- Dry gritty eyes due to reduced blinking. Can last for 2 to 3 weeks. A combination of artificial tears during the day and an ointment at night can help to alleviate dryness. If surgery was done from inside the eyelid, use topical antibiotics, such as chloromycetin, for a week.
- Corneal abrasion (scratched surface of the eye) a minor injury to the eye surface during surgery may cause a small abrasion and pain that lasts for 24 hours. Patients should inform the oculoplastic surgeon if it persists.
- Wound infection may occur during the first 7 to 10 days after blepharoplasty surgery.
- Asymmetry uneven markings may cause swelling due to minimally uneven skin creases or lid height. If the swelling continues for 3 weeks, correct it with another surgery.
- Marked bruising (hematoma) Marked eyelid bruising may occur. Bleeding behind the eye, however, is usually hidden and characterized by severe pain. This may cause loss of vision if not corrected urgently by lateral canthotomy and cantholysis.
- Incomplete eyelid closure for 1 or 2 days, the eyelids may feel stiff and unable to completely cover the whole surface of the eye. This should settle in a few days. If the problem persists, there is a concern of the removal of excess skin.
- Scarring a rare occurrence in the periocular area. It should be revised with “Z-plasty” type surgery to break up and conceal the scar.
- Maintenance surgery if the desired result is not achieved, further surgery may be scheduled.
Results of Upper Eyelid Blepharoplasty
As stated before, each result differs according to the individual’s eyelids and expectations. Before, the eyelids may exhibit wrinkles or orbital fat prolapse, and may cause issues with vision.
After the surgery, the wrinkles on the eyelids should be fully eliminated. The eyelids should open with better positioning and fewer visual problems.
In most cases, photographic analysis and a satisfaction questionnaire after the surgery have shown satisfactory, if not impressive, results often associated with Sculptra treatment. Although this procedure can be offered by plastic surgeons and maxillofacial surgeons, only trained ophthalmologists or oculoplastic surgeons can promise optimum outcomes. This is because they have deep knowledge of the eye’s anatomy and know how to best manage surgical complications.